How fungal infections cause blood poisoning
Blood poisoning caused by a fungal infection is a severe, life-threatening condition. Researchers at the University of Bern have now discovered a mechanism that helps a yeast fungus to spread more easily within the body. The immune system, of all things, plays a major role in this process. These findings could open up new therapeutic avenues for blood poisoning caused by yeast, but also for other invasive fungal infections.
Normally, the yeast Candida albicans is a harmless co-inhabitant of our mucous membranes. About half of the population is colonized by it without noticing. As long as the body's immune system is intact, it effortlessly keeps the fungus in check. It becomes dangerous when the immune system is weakened. This can be the case, for example, with diseases such as AIDS or when taking medication that suppresses the immune defense. In people with a healthy immune system, surgical procedures that damage the mucosal barrier, among other things, can favor the spread of Candida albicans. Once the yeast fungus enters the bloodstream, it can cause blood poisoning (sepsis), leading to permanent damage to internal organs: One-third to one-half of patients do not survive such fungal sepsis.
The natural response of the immune system to the invasion of pathogens is an inflammatory reaction. Sophisticated control mechanisms ensure that only invaders are fought without attacking healthy tissue at the same time. A key role is played by a specific protein, the so-called interleukin 1 receptor antagonist. This protein is the natural antagonist of the pro-inflammatory signal substance interleukin 1, preventing it from overshooting the target and triggering uncontrolled inflammatory reactions.
Inflammation inhibitor weakens immune defense
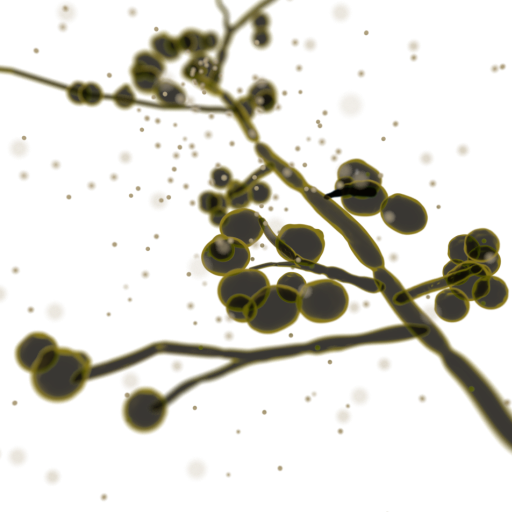
A new study led by Stefan Freigang of the Institute of Tissue Medicine and Pathology (IGMP) at the University of Bern now suggests that the interleukin 1 receptor antagonist (IL-1Ra), despite its anti-inflammatory function, contributes to the spread of Candida albicans. In this context, IL-1Ra produced by the so-called phagocytes (macrophages) seem to be of particular importance. In mice, the researchers were able to show that the amount of those anti-inflammatory proteins in the macrophages increased when Candida albicans entered the bloodstream, and that they subsequently interfered with the immune defense. They inhibited the production and swarming of neutrophils, a subgroup of white blood cells. Neutrophils form an important early barrier against infection by regularly patrolling blood vessels to clear invading pathogens.
Mice genetically bred so that their phagocytes no longer produced the anti-inflammatory proteins had an intact arsenal of neutrophils. Accordingly, they were able to successfully fight an infection with Candida albicans within a short time. In the control group of normal mice, on the other hand, which produced the anti-inflammatory protein, the fungi were able to spread because of the inhibited neutrophils.
Interestingly, the loss of the anti-inflammatory proteins did not lead to an overshooting of the inflammatory response, as would have been expected, but to a reduction. "We explain this by the fact that there were enough neutrophils to eliminate the yeast fungus before it could even trigger a pathogenic inflammatory response," says Stefan Freigang.
So if fewer anti-inflammatory proteins are produced, the neutrophils as the "first line of defense" can do their work undisturbed. However, if the proteins are produced by the phagocytes, this weakens the immune defense. Such complex and dynamic interactions of the immune system can only be mapped in a living organism, which in this case requires animal experiments with genetically modified and normal mice as a control group.
Possible therapeutic approach
The research results of the Bernese researchers could enable new therapeutic approaches in the future. "Fungal sepsis remains difficult to treat and is associated with a high mortality rate. In order to develop more effective treatment strategies, we need a better understanding of the underlying disease mechanisms," explains Stefan Freigang.
In a next step, the researchers want to use samples from patients to confirm the observations from the mouse model and investigate whether the specific protein also promotes infections with Candida albicans in humans. "If this is confirmed, agents targeting the protein could be used as a new strategy to combat the yeast and possibly other fungal infections," Freigang said.
The research findings were published in the journal Immunity.
Publication details:Hang Thi Thuy Gander-Bui, Joëlle Schläfli, Johanna Baumgartner, Sabrina Walthert, Vera Genitsch, Geert van Geest, José A. Galván, Carmen Cardozo, Cristina Graham Martinez, Mona Grans, Sabine Muth, Rémy Bruggmann, Hans Christian Probst, Cem Gabay, Stefan Freigang: Targeted removal of macrophage-secreted interleukin-1 receptor antagonist protects against lethal Candida albicans sepsis. Immunity, 8. August 2023, https://doi.org/10.1016/j.immuni.2023.06.023 |
Institute for Tissue Medicine and PathologyThe Institute of Tissue Medicine and Pathology (IGMP) of the University of Bern covers the entire width of morphological and molecular diagnostics on tissue samples. The combination of service, teaching and research under one roof allows for close interaction and mutual inspiration. Research deals with the development, diagnosis and treatment of diseases. Immune pathologies, inflammatory diseases and aspects of tumor biology are the current research interests. As a university center for tissue medicine and pathology, the IGMP offers the entire spectrum of tissue examinations. Contact persons are defined for each medical field and are well connected in the corresponding interdisciplinary environment. |
2023/08/31